Students and community members learned about the complex history, evolution and future of long-term health care in a talk by a public health expert from Syracuse University.
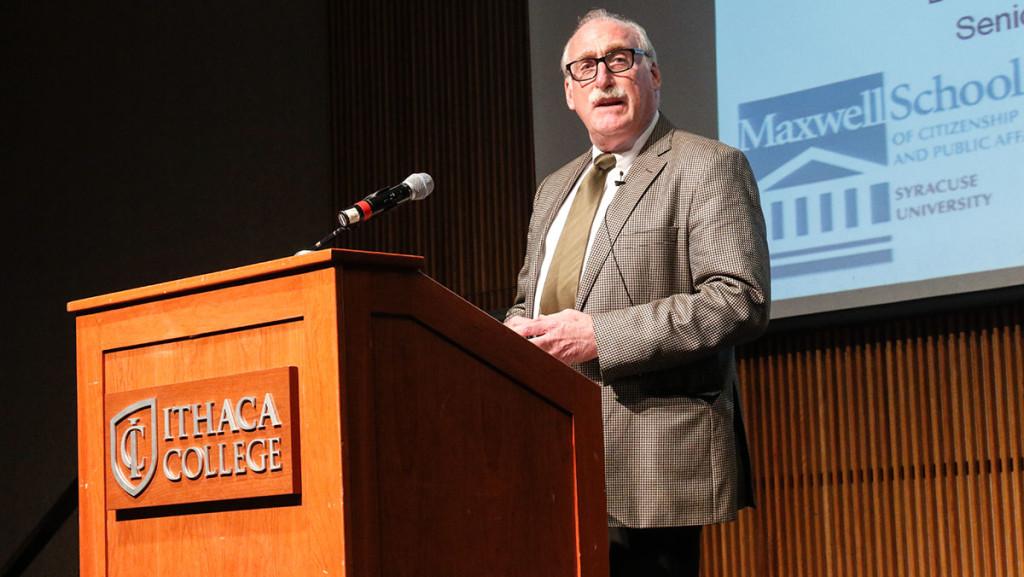
Thomas Dennison is a professor of practice, public administration and international affairs at Syracuse and is also the director of the university’s program in Health Services Management and Policy. Approximately 75 Ithaca College students and Ithaca community members attended the event, which was held Feb. 23 in Emerson Suites.
The event was sponsored by the college’s Gerontology Institute as part of the Gerontology Distinguished Speaker Series, which the college’s website states is held to keep “the college and the … region informed of issues important to elders and professionals who work with and for them.”
The majority of the audience was composed of older adults dealing with or interested in the health care system, and the rest were students who were there to learn how to fix it. Dennison said it is important for people of all ages to learn as much as they can about long-term health care.
“It’s going to happen to you,” he said. “It’s going to happen to your parents. It’s going to happen to your grandparents. The more knowledgeable you are, the more you are able to prepare for yourself but also help other people navigate the system.”
Dennison began his talk with the history of health care. He started at the beginning — England in the 1530s — and covered everything up to the introduction of Social Security, Medicaid and Medicare before moving onto the current long-term care system.
He talked about the decreasing number of older adults deciding to live in nursing homes in conjunction with the growing number of short-term, younger residents of nursing homes and a recent shift to community-based care.
“If you’re going into gerontology in the future, these are the kind of challenges that you’re going to have to face,” he said. “You’re going to have to figure out how to balance the needs of different kinds of individuals.”
He emphasized the discrepancies between the people’s needs and the ability of the government to create programs that meet those needs.
“If you think about a continuum of care, there’s a legal lurch from service based on what resources they have available or what service they can give to the community,” Dennison said.
Dennison also talked about how nonprofit organizations are shown to be providing better overall care than for-profit organizations and about growing competition between nursing facilities. He ended on a positive note, asking students to take on the task of straightening out the health care system.
Sophomore Katharina Dubyk said she enjoyed the event and was particularly fascinated by the trends regarding the ages of nursing home residents.
“I thought it was interesting that in the nursing homes, there are more younger people instead of older people,” Dubyk said. “I’m in an Intro to Aging class, and we learned about the baby boomers, so I thought the number would start increasing.”
Teri Reinemann, gerontology programs manager, said she was “very delighted” with the talk. She complimented Dennison’s in-depth knowledge of the subject.
“He’s obviously extremely knowledgeable, and he has experience in the different levels: home care, hospital care, nursing home care,” Reinemann said. “It’s hard to find someone that can really look at the big picture and understand the big picture while also grasping all the big changes that are happening. He did a really good job.”
Phillip Wacker-Hoeflin, 62, and his wife, Eugenia, 76, said they thought the event would be important to attend in part because Phillip’s mother had difficulties with long-term health care toward the end of her life. His mother was diagnosed with congestive heart failure five years before her death and had to also take care of her ailing husband during that time.
“Two of those years, she had absolutely wretched coverage,” Phillip said. “It was just luck that the last year of her life, she had excellent care. The question is, why should it be so difficult? She had the same financial means.”
“We’re getting old,” Eugenia said. “We’re getting to the age where we have to start being involved with one’s health care. It’s really important to know what we’re moving into. We have long-term care, but it looks as if it’s changing.”